June 25th, 2025
Issue #93
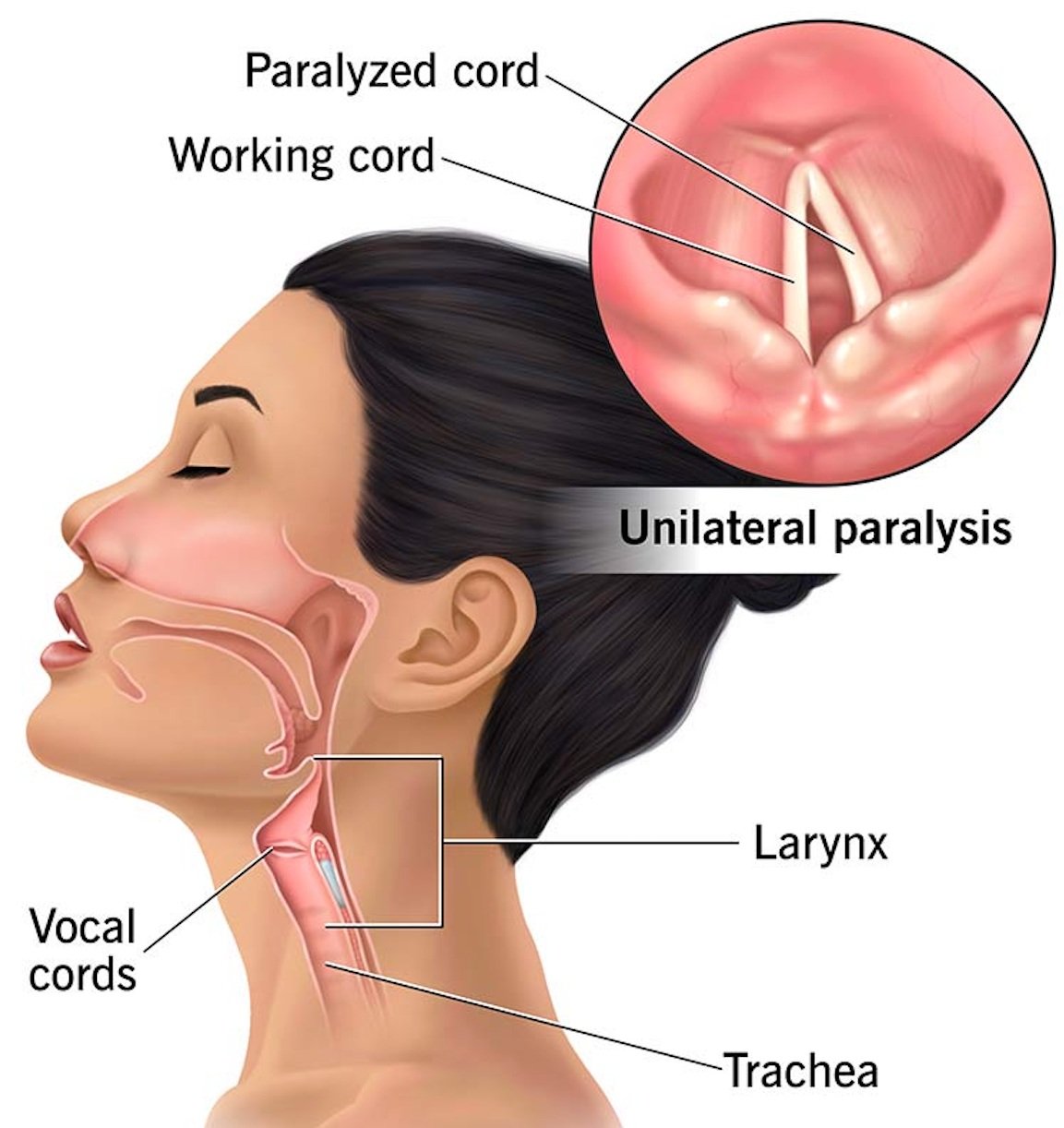
Educational Pearl: Vocal Cord Paralysis
Definition: Loss of movement in one or both true vocal folds due to disrupted motor innervation, most commonly from injury to the recurrent laryngeal nerve, a branch of CN X. This condition affects phonation, airway protection, and respiration, with symptom severity depending on whether one or both vocal cords are affected.
Vocal Cord Paralysis and Associated Anatomy [Image Source]
Key Anatomy:
Recurrent Laryngeal Nerve: Supplies all intrinsic laryngeal muscles except the cricothyroid muscle, which is innervated by the external branch of the superior laryngeal nerve
Posterior Cricoarytenoid Muscle: The only muscle responsible for vocal fold abduction
Other Important Muscles:
Thyroarytenoid
Lateral Cricoarytenoid
Transverse Arytenoid
Oblique Arytenoid
Epidemiology:
Incidence is approximately 1 per 100,000 people per year
More common in females, likely due to higher thyroidectomy rates
Most cases occur between the 5th and 6th decades of life
Unilateral paralysis is more common than bilateral paralysis
Iatrogenic causes, particularly during thyroid and cardiac surgeries, are most frequent in adults
Etiology:
Surgical Injury: Thyroidectomy is one example and the most common cause overall
Malignancy: Tumor-related compression of the recurrent laryngeal nerve
Neurologic Conditions: Examples include stroke and multiple sclerosis
Idiopathic: Often presumed to result from post-viral inflammation affecting the nerve
Clinical Presentation:
Unilateral Paralysis: Hoarseness, breathy voice, mild dysphagia
Bilateral Paralysis: Stridor, dyspnea, weak voice, risk of airway obstruction
Both Types: Aspiration due to incomplete glottic closure
Diagnosis:
Laryngoscopy: The gold standard for confirming vocal fold immobility
Voice Analysis: Shows reduced vocal intensity and pitch range, with increased jitter and shimmer
Imaging with CT or MRI: Recommended if the underlying cause is unclear, especially to rule out malignancy along the course of the nerve
Management:
Unilateral Paralysis:
Voice Therapy: Focuses on strengthening vocal fold movement and improving breath support
Injection Laryngoplasty: Injection of filler material into the paralyzed vocal cord to improve closure
Medialization Thyroplasty: Implant placement to reposition the paralyzed vocal fold
Bilateral Paralysis:
Airway Management: May require a tracheostomy or surgical cord lateralization to maintain an open airway
Visualizing Normal Vocal Cord Movement with Laryngoscopy [Image Source]
Further Readings:
Educational Pearl written by Wid Alhassani
Morsani College of Medicine
Sources:
[1] Masroor F, Pan DR, Wei JC, Ritterman Weintraub ML, Jiang N. The Incidence and Recovery Rate of Idiopathic Vocal Fold Paralysis: A Population-Based Study. Eur Arch Otorhinolaryngol. 2019 Jan;276(1):153-158. Epub 2018 Nov 15. [Article Link]
[2] Cleveland Clinic. Vocal Cord Paralysis. Cleveland Clinic. Published November 16, 2022. Accessed May 28, May 2025. [Image Link]
[3] Mayo Foundation for Medical Education and Research. Vocal Cord Paralysis. Mayo Clinic. Accessed May 28, 2025. [Image Link]
Question of the Week
A 16-year-old male with no significant medical or surgical history presents for evaluation of right-sided nasal congestion and intermittent nosebleeds over the past 4 months. The congestion has progressively worsened and is now constant. He also reports occasional dull right-sided headaches, morning dry mouth, decreased energy, and shortness of breath during weekly soccer practice. He denies fever, chills, or nasal drainage. Over-the-counter antihistamines and nasal sprays have not provided symptomatic relief. The patient is afebrile, and vital signs are within normal limits (BP 112/70 mmHg, HR 84 bpm, RR 14, SpO₂ 99% on room air). He appears pale. Lab values obtained on the day of evaluation are listed below.
Anterior rhinoscopy shows mild right nasal mucosal edema. Flexible nasal endoscopy reveals a smooth, submucosal bulge along the posterior lateral wall of the right nasal cavity, without drainage or bleeding. Which of the following is the most appropriate next step in management for this patient?
(A) Order non-contrast CT of maxillofacial region to evaluate the sinuses
(B) Initiate nasal corticosteroids and reassess in 4 to 6 weeks
(C) Order contrast-enhanced CT and MRI of the head & neck to evaluate the nasal cavity
(D) Schedule in-office biopsy to rule out lymphoma or inverted papilloma
(E) Prescribe empiric oral antibiotics for chronic bacterial rhinosinusitis
Question of the Week written by Luke Reardon
Lincoln Memorial University DeBusk College of Osteopathic Medicine
Looking for the Question of the Week answer and explanation?
· · · · · · · · ·
You’ll find it at the bottom of this newsletter!
Our faculty reviewers have been instrumental in ensuring that we continue to share high-quality content.
We thank them for their contributions to the Auricle!
Facial Plastics and Reconstruction
Dr. Leslie Kim, MD, MPH
The Ohio State University Wexner Medical Center
Head and Neck
Dr. Michael Topf, MD
Vanderbilt University Medical Center
Pediatric Otolaryngology
Dr. Michele Carr, MD, DDS, PhD
Jacobs School of Medicine and Biomedical Sciences, University at Buffalo
Rhinology and Skull Base Surgery
Dr. Christina Fang, MD
Montefiore Medical Center
Medical Student Feature Series
Editor’s Note: The Auricle is proud to share the recurring section below, highlighting recently published student-led research in top ENT journals with medical students as first authors. The Medical Student Feature Series celebrates the outstanding scholarship and contributions of future otolaryngologists.
Please join us in celebrating our peers and learning from their achievements!
Tracheostomy Techniques in Severe COVID-19: Open vs. Percutaneous Approaches
Dobbin ML, Bernard A, Pyle L, et al. Comparison of WatchPAT to Polysomnography Measurement of Apnea-Hypopnea Index and Obstructive Sleep Apnea Severity in Adolescents with Overweight and Obesity. J Clin Sleep Med. 2025 Apr 1;21(4):695-702. [Article Link]
False alarms in the fight against adolescent obstructive sleep apnea
Overweight and obese adolescents are at significantly increased risk for obstructive sleep apnea (OSA), yet access to in-lab polysomnography (PSG) remains limited. This prospective study evaluated 38 patients aged 10 to 21 years (mean age 15.5 ± 1.6 years), all with a body mass index at or above the 85th percentile for age and sex, who were referred for PSG due to concern for possible OSA. Each participant underwent both PSG and WatchPAT, a peripheral arterial tonometry–based device. WatchPAT overestimated the apnea-hypopnea index by an average of 16.9 ± 13.4 events per hour (95% confidence interval 12.5 to 21.3) and accurately classified OSA severity in only 4 of 38 cases (10.5%). Sensitivity declined with increasing OSA severity, dropping from 100.0% in mild cases to 62.0% in severe cases, while specificity increased from 5.5% in mild OSA to 100.0% in severe OSA, highlighting inconsistent diagnostic performance and undermining overall reliability. Although PSG underestimation contributed to discrepancies in a few cases, the authors suggest that physiological differences in adolescents may interfere with WatchPAT’s adult-calibrated algorithm. These findings indicate that WatchPAT may not be a reliable tool for diagnosing OSA in this high-risk population.
Summary written by Rushi Vekariya
University of Central Florida College of Medicine
Have you recently published a first-author article as a medical student?
E-mail theauricleotolaryngology@gmail.com to be featured in our newsletter!
Mia Dobbin
Rocky Vista University College of Osteopathic Medicine
Class of 2025
Facial Plastic and Reconstructive Surgery
Free Muscle Flap Transfer for Facial Reanimation: Review and Meta-Analysis
Zhang J, Ye X, Zhang Y, Sun C, Pang P. Free Muscle Flap Transfer for Facial Reanimation: A Systematic Review and Meta-Analysis. Laryngoscope. 2025 May 1. Online ahead of print. [Article Link]
Are certain muscle-nerve pairings more effective for facial reanimation?
Free muscle flap transfer (FMFT) is a well-established technique for restoring facial movement and symmetry in patients with long-standing facial paralysis. This systematic review and meta-analysis included 48 and 25 retrospective studies, respectively, encompassing 1747 patients who underwent 1930 FMFTs to evaluate the effectiveness of various muscle–nerve pairings. The gracilis muscle was the most commonly used donor flap (n = 1245, 64.5%), most flaps were single innervated rather than double (n = 1722, 89.2% vs n = 208, 10.8%), and the most common single innervation source was the masseteric nerve (n = 751, 38.9%) applied on the paralyzed side. Postoperative outcomes across 15 (60.0%) studies showed significant improvement in facial nerve function on the paralyzed side, with a total postoperative increase in oral commissure movement of 8.2 mm (95% confidence interval [CI] 6.3 to 10.0; p < 0.00001) and no evidence of publication bias (p = 0.669). Overall facial movement, coordination, and symmetry improved significantly, with Terzis-Noah and House-Brackmann scores increasing by 2.35 (95% CI 1.64 to 3.05; p < 0.00001) and decreasing by -2.59 (95% CI -3.04 to -2.13; p < 0.00001), respectively, and oral commissure asymmetry decreasing by 7.42 mm (95% CI -8.38 to -6.45; p < 0.00001), despite a residual asymmetry of 3.45 mm remaining postoperatively (95% CI 1.48 to 5.43; p = 0.0006). Quality of life also improved significantly, with the mean Facial Clinimetric Evaluation Scale questionnaire score increasing by 18.2 points postoperatively (95% CI 13.4 to 23.1; p < 0.00001) across five studies (20.0%). The authors conclude that FMFT is a highly effective treatment, with nerve-flap selection best guided by patient anatomy and clinical context.
Summary written by Chinelo Eruchalu
Jacobs School of Medicine and Biomedical Sciences, University at Buffalo
Head and Neck
Face and Neck Pilomatricoma Excision Using an Endoscope-Assisted Hairline Approach
Woo K, Lee DK, Woo SH. Face and Neck Pilomatricoma Excision Using an Endoscope-Assisted Hairline Approach. OTO Open. 2025 May 15;9(2):e70104. eCollection 2025 Apr-Jun. [Article Link]
Hidden incisions, visible results
Pilomatricomas are benign tumors originating from hair follicles that are typically treated with surgical excision, though this can result in visible scarring. An endoscope-assisted hairline approach allows for precise tumor removal within a controlled field while improving cosmetic outcomes by concealing the incision within the hairline. This prospective observational study compared outcomes in 50 patients with pilomatricomas, 25 of whom underwent traditional excision and 25 who received the endoscope-assisted hairline technique. Cosmetic outcomes were assessed using standardized photographs and patient satisfaction scores at both 3 and 12 months postoperatively. The endoscopic approach was associated with a significantly longer operative time (85.6 ± 37.2 minutes) compared to the conventional method (49.2 ± 14.1 minutes; p < 0.001). However, patients treated with the endoscopic technique reported significantly higher cosmetic satisfaction scores (9.9 ± 0.4 vs. 7.3 ± 1.1; p < 0.001), and objective evaluations showed reduced scar visibility and improved preservation of skin appearance. The endoscope-assisted hairline approach for excising head and neck pilomatricomas represents a meaningful surgical advancement, offering improved aesthetic outcomes through hidden incisions, enhanced visualization, and complete tumor removal with minimal tissue disruption.
Summary written by Anders Erickson
Des Moines University College of Osteopathic Medicine
Laryngology
Non-Phonatory Voice Therapy for Post-Thyroidectomy Unilateral Vocal Fold Paralysis
Longobardi Y, Mari G, Libero R, et al. Effects of Early Voice Therapy Intervention Using Non-Phonatory Exercises in Patients with Unilateral Vocal Fold Paralysis After Thyroidectomy: A Randomized Clinical Trial. J Voice. 2025 May 5:S0892-1997(25)00169-9. Online ahead of print. [Article Link]
Silent exercises speak volumes.
Iatrogenic unilateral vocal fold paralysis (UVFP) following thyroid surgery, often caused by recurrent laryngeal nerve injury, can significantly impair voice quality and overall quality of life. This randomized clinical trial investigated whether early intervention with non-phonatory exercises (NPEs) improves outcomes in patients with iatrogenic UVFP. A total of 20 adult patients diagnosed with UVFP post-thyroidectomy were recruited between February 2024 and September 2024 and randomized to receive either cortisone plus one week of NPEs (group A, n = 10, 50.0%) or cortisone alone (group B, n = 10, 50.0%), followed by standard voice therapy for all participants. At one week post-intervention, group A showed significantly greater improvements in incomplete glottal closure (p = 0.001), incomplete membranous vocal cord closure (p = 0.04), complete glottal closure (p = 0.001), and phonation duration (p < 0.05) compared to group B. After five additional sessions of standard voice therapy, group A also demonstrated significantly lower minimum voice frequencies (p = 0.005) and improved scores for instability (p = 0.02) and breathiness (p = 0.03). Some acoustic measures, including jitter (pitch variation) and shimmer (amplitude variation), decreased significantly over time (p = 0.001 and p = 0.01, respectively) regardless of intervention. These findings suggest that early use of NPEs may improve vocal cord function and voice outcomes in post-thyroidectomy patients with iatrogenic UVFP.
Summary written by Anuhya Kanchibhatla
Case Western Reserve University School of Medicine
Otology and Neurotology
Statin Use and Reduced Risk of Sudden Sensorineural Hearing Loss in Type 2 Diabetes
Li TH, Shiu JS, Chen WM, Shia BC, Wu SY, Lin HC. Statin Use and Reduced Risk of Sudden Sensorineural Hearing Loss in Type 2 Diabetes. Otolaryngol Head Neck Surg. 2025 Mar 24. Online ahead of print. [Article Link]
Sudden sensorineural hearing loss (SSNHL) is an otolaryngologic emergency defined as a rapid, often unexplained decline in hearing that has been associated with metabolic conditions such as type 2 diabetes mellitus (T2DM), possibly due to microvascular, inflammatory, or autoimmune mechanisms affecting the cochlea. Given the profound impact of SSNHL on communication and social functioning, this study aimed to clarify the relationship between T2DM and the risk of developing SSNHL. In this nationwide retrospective cohort study, patients diagnosed with T2DM between January 1, 2008, and December 31, 2019, were identified from Taiwan’s National Health Insurance Database and categorized based on statin use. A total of 66,120 patients (50.0%) received statins as lipid-lowering therapy, while 66,120 (50.0%) did not. Statin use was associated with a significantly lower risk of developing SSNHL, with an adjusted hazard ratio (aHR) of 0.83 (95% confidence interval [CI] 0.74 to 0.92; p = 0.0008), and with reduced all-cause mortality (aHR = 0.55; 95% CI 0.52 to 0.57; p < 0.0001). A dose-dependent effect was also observed, with higher daily statin doses correlating with progressively lower SSNHL risk. These findings suggest that statin therapy may reduce the risk of SSNHL and offer potential otoprotective benefits for patients with T2DM.
Summary written by Maaz Haji
Chicago Medical School, Rosalind Franklin University
Pediatric Otolaryngology
Randomized Clinical Trial of Non-Opioid Pain Medications After Intracapsular Adenotonsillectomy
Lu NE, Shaffer AD, Rushchak MV, et al. Randomized Clinical Trial of Non-Opioid Pain Medications After Intracapsular Adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2025 Jun:193:112361. [Article Link]
Post-adenotonsillectomy pain control: Are Acetaminophen and Ibuprofen enough?
Pediatric tonsillectomies account for over 50% of opioid prescriptions in the United States, emphasizing the need for effective non-opioid postoperative pain management. In this randomized, open-label, controlled trial, 70 pediatric patients aged 3 to 17 who underwent intracapsular adenotonsillectomy (T&A) at a single tertiary children’s hospital between April 2021 and May 2023 were divided into two groups by opioid use (opioid: n = 36, 51.4% vs. non-opioid: n = 34, 48.6%) and followed over the first 14 postoperative days. All patients were permitted to use acetaminophen and ibuprofen, but only those in the opioid group received oxycodone prescriptions for additional analgesia. Using the validated Wong-Baker FACES Pain Rating Scale, the study authors found no significant differences in postoperative average pain scores before analgesia (3.2, 95% confidence interval [CI] 2.5 to 3.8 vs. 3.3, 95% CI 2.5 to 4.0) or after analgesia (1.1, 95% CI 0.5 to 1.5 vs. 1.0, 95% CI 0.5 to 1.5). In addition, only 33.3% (n = 7) of the 21 opioid group patients who completed follow-up consumed one or more oxycodone doses, and no patients in the non-opioid group (0.0%) requested or received opioids. No significant differences were observed in average peak pain before (7.7, 95% CI 6.8 to 8.6 vs. 7.4, 95% CI 6.5 to 8.4) or after analgesia (3.8, 95% CI 2.6 to 4.9 vs. 3.6, 95% CI 2.4 to 4.8), analgesic use duration (9.5 ± 2.8 days vs. 9.5 ± 3.6 days; p = 0.96), or total analgesic doses (40.1 ± 18.8 doses vs. 43.2 ± 21.7 doses; p = 0.6). However, the generalizability of these findings is limited by low sample size and loss to follow-up.
Summary written by Michelle Nguyen
Edward Via College of Osteopathic Medicine - Virginia
Rhinology and Skull Base Surgery
Olfactory Deficits and Mortality in Older Adults
Ruane R, Lampert O, Larsson M, Vetrano DL, Laukka EJ, Ekström I. Olfactory Deficits and Mortality in Older Adults. JAMA Otolaryngol Head Neck Surg. 2025 Jun 1;151(6):558-566. [Article Link]
Sniffing out mortality risk factors
Olfactory impairment has been associated with increased mortality, but the underlying mechanisms remain unclear. This population-based, longitudinal cohort study included 2,524 adults (mean age 71.9 ± 10.0 years) from the Swedish National Study on Aging and Care in Kungsholmen, an ongoing study of residents aged 60 years or older in Stockholm, Sweden, enrolled between 2001 and 2004. Participants younger than 78 years were followed every six years, and those 78 or older were followed every three years, with the 12-year follow-up completed in 2013. Olfactory function was assessed using the 16-item Sniffin’ Sticks Odor Identification task. Each incorrect response was associated with a 6% increase in six-year mortality (hazard ratio [HR] = 1.06; 95% confidence interval [CI] 1.03 to 1.09) and a 5% increase in 12-year mortality (HR = 1.05; 95% CI 1.03 to 1.08). In cause-specific models, the association between olfactory dysfunction and mortality was strongest for neurodegenerative deaths at both six and 12 years (HR = 1.28; 95% CI 1.18 to 1.38 and HR = 1.19; 95% CI 1.13 to 1.25, respectively), with key mediators being dementia, frailty, and malnutrition. These findings suggest that olfactory impairment may serve as a marker of elevated mortality risk and reflect underlying neuroinflammation, genetic changes, immune dysfunction, or vascular burden contributing to physical decline.
Brooke Swain’s Takeaway: Given the extensive olfactory pathway from nasal chemoreceptors to the olfactory cortex, further research is needed to determine whether the association between olfaction loss and mortality stems from deficits in downstream integrative processing. Other sensory impairments, such as hearing loss or vestibular dysfunction, might also serve as parallel markers of mortality risk.
Summary written by Brooke Swain
Vanderbilt University School of Medicine
Sleep Surgery
Backscattered Ultrasonographic Imaging and Outcomes in Hypoglossal Nerve Stimulation
Tschopp S, Janjic V, Lee Y, et al. Backscattered Ultrasonographic Imaging of the Tongue and Outcome in Hypoglossal Nerve Stimulation. Otolaryngol Head Neck Surg. 2025;172(6):2134-2140. [Article Link]
Radiology rules the world: Predicting HGNS outcomes with ultrasound
Hypoglossal nerve stimulation (HGNS) is an emerging surgical treatment for obstructive sleep apnea (OSA) in patients who cannot tolerate continuous positive airway pressure (CPAP) therapy, but accurately identifying suitable surgical candidates for HGNS implantation remains a clinical challenge. In this multi-center cross-sectional study, 65 adults with OSA refractory to CPAP or mandibular advancement devices underwent HGNS implantation followed by standardized submental ultrasonographic examination and postoperative home sleep apnea testing. Submental ultrasonography, which uses a robotic arm for consistent positioning, was utilized to assess the upper airway. The two primary outcomes were HGNS response, defined as a postoperative apnea-hypopnea index (AHI) below 20 events per hour and a greater than 50.0% reduction from baseline, and the backscatter ultrasonographic imaging (BUI) value of the posterior tongue, which reflects fat deposition. BUI values were moderately higher in patients who did not respond to HGNS, both in a region corresponding to the velum (r = 0.35, 95% CI 0.12 to 0.58; median difference = 0.05, 95% CI 0.02 to 0.08) and in a region corresponding to the oropharynx (r = 0.30, 95% CI 0.05 to 0.52; median difference = 0.03, 95% CI 0.01 to 0.06). Using baseline AHI alone with a threshold of ≤ 39 events per hour, the average prediction accuracy for HGNS response was 71.3% with a specificity of 69.4%, compared to 77.1% accuracy and 88.9% specificity when BUI values were combined with AHI. The authors concluded that incorporating BUI with AHI improves the ability to predict HGNS response among surgical candidates.
Matthaeus Hendricks’ Takeaway: The potential role of ultrasound in predicting HGNS response is encouraging, but post-implantation imaging assumes no treatment-related changes in oropharyngeal fat composition. Pre-implantation BUI assessment and evaluation of additional oropharyngeal sites may strengthen the tool’s predictive value.
Summary written by Matthaeus Hendricks
Jacobs School of Medicine and Biomedical Sciences, University at Buffalo
Basic Science Spotlight
Postoperative ctHPVDNA Kinetics in HPV-Related Oropharyngeal Cancer
Yin LX, Hidalgo CM, Bogan AW, et al. Postoperative ctHPVDNA Kinetics in Patients with HPV-Related Oropharyngeal Cancer. JAMA Otolaryngol Head Neck Surg. Published online May 14, 2025. [Article Link]
Can ctHPVDNA guide the need for adjuvant therapy?
Circulating tumor human papillomavirus (HPV) DNA (ctHPVDNA) has recently gained attention as a screening tool for HPV-related cancers, particularly for monitoring treatment response and detecting residual disease. While current standards of care rely heavily on tumor pathologic characteristics to guide adjuvant therapy, the morbidity associated with these treatments highlights a need for additional quantifiable risk factors to ensure they are reserved for cases where resection is non-curative. In this prospective study, 57 patients with HPV-related oropharyngeal cancer scheduled for curative surgery with neck dissection underwent blood sampling to assess ctHPVDNA levels at multiple pre- and postoperative time points. Preoperative levels of tumor tissue-modified viral (TTMV) ctHPVDNA were significantly associated with nodal involvement, including the size of the largest node (odds ratio [OR] = 2.51; 95% confidence interval [CI] 1.25 to 6.21) and the number of involved lymph nodes (OR = 1.86; 95% CI 1.08 to 3.94). Additionally, TTMV ctHPVDNA measured on postoperative days 1 to 2 correlated with the number of involved lymph nodes (OR = 1.37; 95% CI 1.05 to 1.87) and showed a mild association with pathologic T stage (η2 = 0.06; 95% CI 0.01 to 0.28). Importantly, TTMV ctHPVDNA on postoperative day 1 demonstrated a low positive predictive value for week 2 levels (0.19; 95% CI 0.04 to 0.46), but a high negative predictive value (0.95; 95% CI 0.74 to 1.00). These findings suggest that early postoperative TTMV ctHPVDNA negativity may reflect persistently low subclinical levels, though further studies are needed to determine the optimal sampling window to guide adjuvant treatment decisions.
Summary written by Emily Chestnut
Indiana University School of Medicine
Question of the Week Answer
Correct Answer: (C) Order contrast-enhanced CT and MRI of the head & neck to evaluate the nasal cavity
Answer Explanation:
This adolescent male presents with progressive unilateral nasal obstruction, intermittent epistaxis, waking with a dry mouth (suggestive of mouth-breathing), and anemia, all of which point toward a diagnosis of juvenile nasopharyngeal angiofibroma (JNA). His exam reveals posterior nasal cavity fullness and labs confirm chronic blood loss. Despite a relatively nonspecific anterior rhinoscopy, these findings warrant further evaluation with contrast-enhanced imaging before any therapy is initiated.
Contrast-enhanced CT of the head & neck is essential to evaluate for bony remodeling or erosion of the pterygoid plates and adjacent skull base structures, which are commonly involved in JNA. MRI with contrast complements CT by delineating soft tissue extension into the nasopharynx, pterygopalatine fossa, orbit, or intracranial cavity, all of which are critical features for JNA staging and surgical planning. Together, these imaging modalities provide the anatomical detail needed to confirm a JNA diagnosis and guide safe management.
Answer choice (A), ordering non-contrast CT to evaluate the sinuses, would not adequately evaluate the tumor's vasculature or delineate soft tissue involvement, both of which are essential in the workup of suspected JNA. Answer choice (B), initiating nasal corticosteroids, might reduce nasal congestion but would not address the underlying tumor and may delay definitive diagnosis and management. Answer choice (D), performing a biopsy, is contraindicated in this context due to the high risk of hemorrhage associated with vascular tumors like a JNA. Answer choice (E), prescribing antibiotics for bacterial rhinosinusitis, is inappropriate because this patient has no clinical signs of infection such as purulence, fever, or facial tenderness.
Question of the Week Answer written by Luke Reardon
Lincoln Memorial University DeBusk College of Osteopathic Medicine
Sources:
[1] 4th ed. Plural Publishing; 2014. Otolaryngology Head and Neck Surgery: Clinical Reference Guide.Pasha R, Golub JS.
[2] American Academy of Otolaryngology–Head and Neck Surgery Foundation. Primary Care Otolaryngology Handbook. 4th ed. American Academy of Otolaryngology–Head and Neck Surgery Foundation; 2019.
Copyright © 2024, All rights reserved. Images used in this newsletter remain the property of their creators and/or publishing organization but are reprinted here for educational use.
The Auricle Mailing Address: theauricleotolaryngology@gmail.com