The Auricle on Sundays with Saima & Co.
The Auricle on Social Media
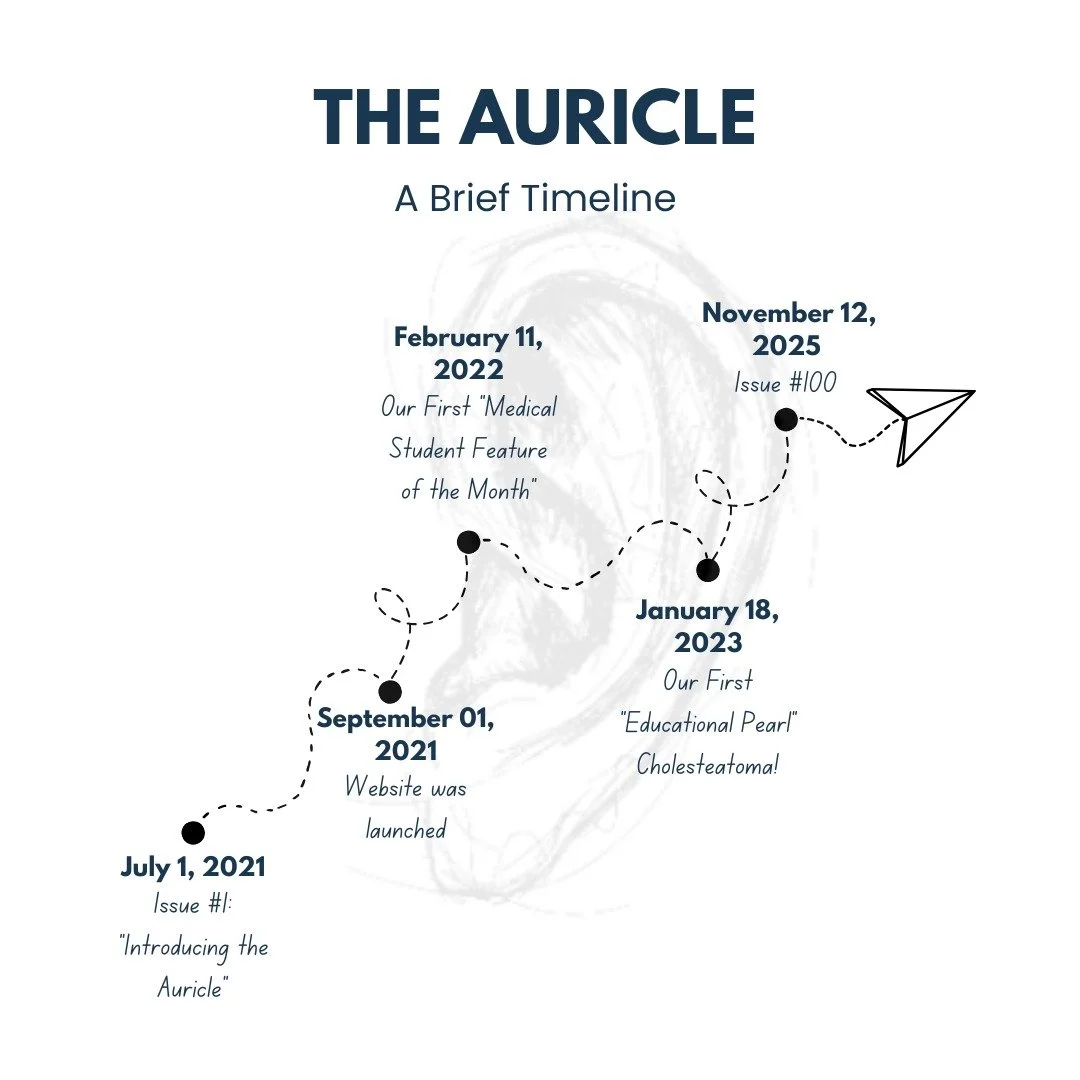
A medical student-run newsletter featuring the latest cutting edge research in otolaryngology — curated by medical students, for medical students
For more otolaryngology content, visit our partner site headmirror.com